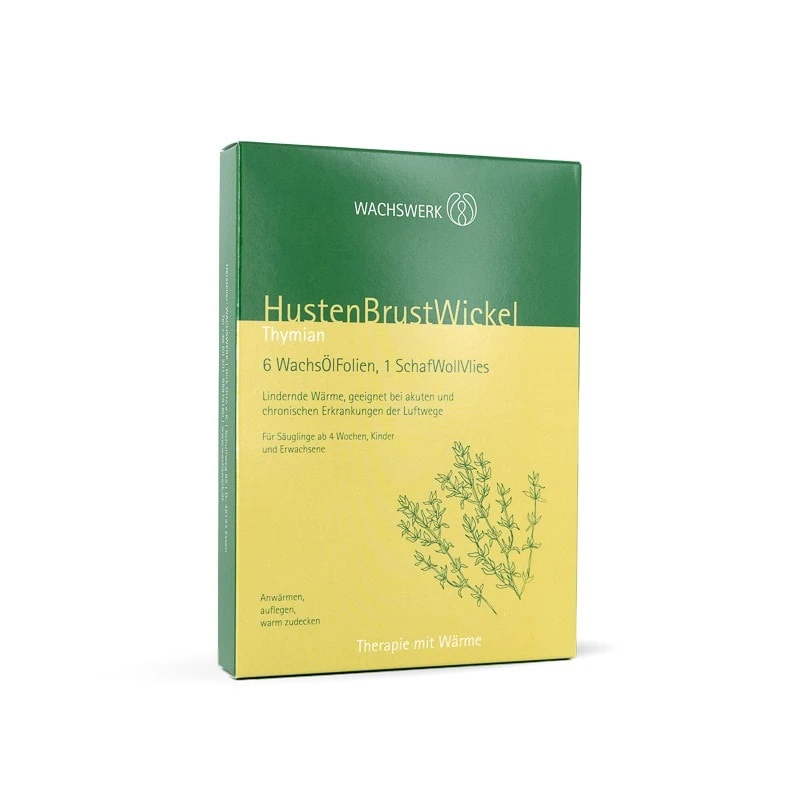
Thyme wax plates application (Wachswerk)
Indication:
Regulation of body heat, respiratory diseases such as bronchitis, bronchiolitis, especially in the case of heavy secretion and mucus in the airways
From what age:
From the 4th week of life
Material
- One sheet of thyme wax
- Wool
- Heat source
Care of the equipment
- Wax sheets are for single use
- The wool can be reused
- Disinfection
*A cherry stone cushion, bed bottle or hairdryer can be used as a heat source
Application
- Thyme wax sheets are heated with a hairdryer or in a crackling bag with a cherry stone cushion or bed bottle
- Thyme wax plates are placed on the child's chest
- Then place a piece of wool over the wax plate. The piece of wool should be larger than the wax plate
- This can be fastened with a bodysuit or undershirt
The wrap is applied for at least 30 minutes, but can also be applied overnight
Thyme wax plates application (Wachswerk) Read More »













